 Henle's loop is a U-shaped structure consisting of a thick descending limb, a thin descending limb, a thin ascending limb and a thick ascending limb. The thin tubules are composed of squamous epithelial cells. The length of the thin segments varies with the location of the nephron. In cortical nephrons, the thin segment is only 1 to 2 mm long or may be completely absent. Juxtamedullary nephrons have thin segments, 9 to 10 mm in length, which form a hairpin-like loop that extends deep into the medulla as far as the renal papilla. It is possible to differentiate among four types of epithelial cells composing different regions of Henle's loop according to their fine structural features [2]. The locations and fine structural features of the four cell types are listed in Table 1.
Henle's loop is a U-shaped structure consisting of a thick descending limb, a thin descending limb, a thin ascending limb and a thick ascending limb. The thin tubules are composed of squamous epithelial cells. The length of the thin segments varies with the location of the nephron. In cortical nephrons, the thin segment is only 1 to 2 mm long or may be completely absent. Juxtamedullary nephrons have thin segments, 9 to 10 mm in length, which form a hairpin-like loop that extends deep into the medulla as far as the renal papilla. It is possible to differentiate among four types of epithelial cells composing different regions of Henle's loop according to their fine structural features [2]. The locations and fine structural features of the four cell types are listed in Table 1.The Distal Convoluted Tubule
The thick ascending limb of Henle's loop penetrates the cortex and is called the distal convoluted tubule (DCT). The DCTs differ from the PCTs in that they have no brush border, no apical canaliculi, and smaller cells.  DCT, like the ascending limb, is lined with simple cuboidal epithelium containing more or less round and apically located nuclei, having one or two dense nucleoli [2]. Cells of the DCTs have elaborate basal membrane invaginations and associated mitochondria indicative of their ion-transporting function [3]. Microvilli are present on the apical surface but they are much fewer in number and shorter than those of the proximal tubule [4]. As the ascending thick limb of the Henle loop passes near its own renal corpuscle, it lies between the afferent and efferent glomerular arterioles.
DCT, like the ascending limb, is lined with simple cuboidal epithelium containing more or less round and apically located nuclei, having one or two dense nucleoli [2]. Cells of the DCTs have elaborate basal membrane invaginations and associated mitochondria indicative of their ion-transporting function [3]. Microvilli are present on the apical surface but they are much fewer in number and shorter than those of the proximal tubule [4]. As the ascending thick limb of the Henle loop passes near its own renal corpuscle, it lies between the afferent and efferent glomerular arterioles. This region of the distal tubule is called the macula densa. The cells of the macula densa are columnar and their nuclei are closely packed together. Most of the cells have a Golgi complex in the basal region. These cells are sensitive to the ionic and water volume of the tubular fluid and lead to the release of the enzyme renin in the circulation [3].
This region of the distal tubule is called the macula densa. The cells of the macula densa are columnar and their nuclei are closely packed together. Most of the cells have a Golgi complex in the basal region. These cells are sensitive to the ionic and water volume of the tubular fluid and lead to the release of the enzyme renin in the circulation [3].
Juxtaglomerular Apparatus
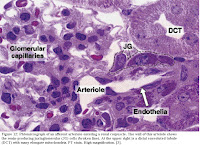 Together, the portion of the afferent arteriole containing the JG cells with the macula densa make up the juxtaglomerular apparatus [2,3]. Extraglomerular mesangial cells are also part of the apparatus and are coupled to one another and to JG cells by gap junctions. They are believed to be involved in transmitting information from the macula densa to JG cells [4]. The macula densa and the JG cells have a special geographical relationship in this area because the internal elastic membrane of the afferent arteriole is not present at this point, allowing intimate contact between cells of the macula densa and the JG cells [2,3].
Together, the portion of the afferent arteriole containing the JG cells with the macula densa make up the juxtaglomerular apparatus [2,3]. Extraglomerular mesangial cells are also part of the apparatus and are coupled to one another and to JG cells by gap junctions. They are believed to be involved in transmitting information from the macula densa to JG cells [4]. The macula densa and the JG cells have a special geographical relationship in this area because the internal elastic membrane of the afferent arteriole is not present at this point, allowing intimate contact between cells of the macula densa and the JG cells [2,3].
Collecting Tubules and Ducts
The collecting tubules are not part of the nephron as they have different embryological origins and only meet the nephron later in development to join it and make a continuous structure [4]. Urine passes from the DCTs to collecting tubules that join each other to form larger, straight collecting ducts which expand progressively as they near the tips of the medullary pyramids[3]. The permeability of collecting ducts is regulated by antidiuretic hormone (ADH). In its absence, such as in times of water excess they are impermeable to water. In its presence, when water in under-consumed, the opposite is true [4]. Collecting ducts are about 20 mm long and have three recognized regions.
1. Cortical collecting tubules are located in the medullary rays and are composed of two types of cubiodal cells: principal cells and intercalated cells. Principal cells have oval, centrally located nuclei and a few small mitochondria. The basal membrane of these cells contains numerous infoldings however do not interdigitate with neighboring cells. The lateral cell membranes are not plicated (folded). Intercalated cells have round, centrally located nuclei and an abundance of mitochondria. The apical cytoplasm contains numerous vesicles. Microplicae (cytoplasmic folds) and microvilli are also present on their apical surface. These cells do not have basal infoldings but do have basally located interdigitations with neighboring cells. Intercalated cells actively transport and secrete hydrogen ions against high concentration gradients and are thus involved in the acid-base balance of the body [2,4]. 2. Medullary collecting tubules are formed by the joining of several cortical collecting tubules and are thus larger than the above. In the outer region of the medulla, meduallry collecting tubules are similar to cortical collecting tubules in that they contain both principal and intercalated cells. Tubules of the inner medulla lack intercalated cells [2].
2. Medullary collecting tubules are formed by the joining of several cortical collecting tubules and are thus larger than the above. In the outer region of the medulla, meduallry collecting tubules are similar to cortical collecting tubules in that they contain both principal and intercalated cells. Tubules of the inner medulla lack intercalated cells [2].
3. Papillary collecting tubules (ducts of Bellini) are formed by the union of several medullary collecting tubules. These larger ducts, lined by tall columnar principal cells, open at the area cribrosa of the renal papilla to deliver the urine they carry into the minor calyx of the kidney [2].
 Calyces
CalycesA minor calyx is a funnel-shaped chamber which accepts urine from the renal papilla of a renal pyramid. The portion of the apex of the pyramid that projects into the minor calyx is covered by transitional epithelium. This type of epithelium separated urine from the underlying interstitial connective tissue, thus acting as a barrier. A muscular coat composed entirely of smooth muscle lies below the lamina propria. This layer forces the urine into a major calyx, a large funnel-shaped chamber, which recieves urine from two to four minor calyces. Major calyces are similar in structure and function to minor calyces and push the urine into the ureter which in turn delivers the urine to the urinary bladder for excretion [2,4].
